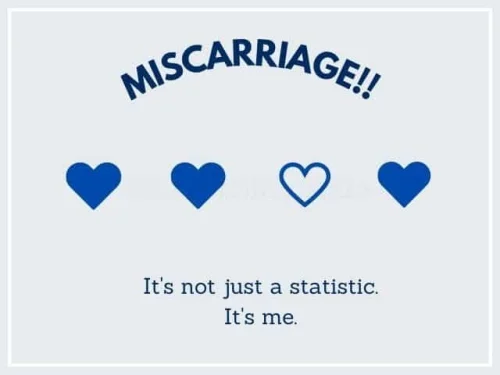
15-20% of all confirmed pregnancies end in miscarriage, according to the data available today.
75% of all miscarriages happen in the first 12 weeks and in many cases, the woman is not even aware that she’s pregnant.
Finding the possible reason for your recurrent pregnancy loss is crucial before deciding on any treatments.
Causes of recurrent early miscarriages (1st trimester)
- Chromosomal Abnormalities - Upto 65% of pregnancy losses are attributed to chromosomal abnormalities in the fetus.There is 50% risk of miscarriage if you get pregnant after 40 because chances of aneuploidy (addition of extra chromosomes) are much higher. In women under 35, the risk of miscarriage is only around 10%, given all other factors are normal.
- Uterine anomalies - 13% of recurrent miscarriage patients are noted to have anomalies in their uterine cavity—arcuate uterus, septate uterus, unicornuate or bicornuate uterus and a didelphys uterus. Septate uterus is the most common abnormality in which the uterus is separated into two by a septum.
- Incompetent cervix - 28% of women with repeated second trimester miscarriages or preterm deliveries were found to have cervical insufficiency. It can normally be managed with cervical cerclage, in which the doctor will place stitches on the cervix to allow it to hold the pregnancy.
Causes of recurrent late miscarriages
- Antiphospholipid syndrome - Antiphospholipid Syndrome (aPL) is an auto-immune disease responsible for recurrent miscarriages in around 10-15% of women. Miscarriage at 10 weeks or more of gestation is more strongly associated with aPL than are earlier pregnancy losses. Testing for antiphospholipid antibodies can be carried out in RPL patients but only after the anatomic, hormonal, and chromosomal causes have been ruled out. If you test positive, Low doses aspirin and heparin are part of treatment regimen.
- Immunologic problems - Reduced maternal immune tolerance towards the fetus is considered one of the causes of repeated miscarriage. Autoantibodies including APA, anticardiolipin antibodies (ACA), and antinuclear antibodies (ANA) have been found to play a role in recurrent pregnancy loss.
- Hormonal and metabolic factors
- Hypothyroidism – Thyroid levels should be evaluated and TSH levels should be below 2.5mIU/L before trying for pregnancy.
- Diabetes – Highly elevated blood sugar can cause loss of pregnancy.
- Endocrine issues – Excessive androgens as in PCOD/PCOS may cause repeated miscarriages.
- Increased prolactin – Elevated prolactin levels hamper follicular development and luteal function. This leads to reduction in progesterone levels in the luteal phase of the cycle. In patients with repeated miscarriage, progesterone supplements can be given to improve their chances of IVF success.
- Thrombophilia (propensity for blood clots) - About 15% of recurrent miscarriages are attributed to blood clotting. If confirmed, an anti-coagulant drug called Heparin will be used to prevent blood clots during your pregnancy.
- Lifestyle factors - Excessive consumption of alcohol, cigarettes and cocaine use have been reported to raise the risk of miscarriage. Researchers found that excessive consumption of caffeine (by both men and women) even during pre-pregnancy could cause miscarriages.
Unexplained repeated miscarriage
In over 50% of patients, clinicians are unable to find the reason for multiple miscarriages. Unexplained recurrent miscarriages are extremely challenging and frustrating but you must know that the chances of a successful pregnancy in these cases are as high as 50-60%. They have excellent prognosis.